In the past, there were only three ways to get out of the kidney transplant waiting list. The first is to find a healthy person from your friends and family, perfectly match the recipient's blood and tissue type, and have a spare kidney that he or she is willing to give up.
The second is to wait for a stranger to die unexpectedly. This stranger is a suitable body match and happens to have checked the organ donation on their driver's license.
The third is death.
But then the doctors thought: With enough kidney patients and enough healthy voluntary donors, they can form a large enough donor pool to promote more matches than the one-to-one system in the past. As long as the patient can find the donor - any donor, even if it does not match the patient itself - they can get a matching kidney.
Initially, this required the doctor to spend several hours carefully studying the blood type and tissue changes in the patient and potential donor list. Then, computer scientists and economists came in. The algorithms they build perform these complex matches more elegantly than the human brain. Now, thanks to artificial intelligence, a person who takes the courage to take a step to donate a kidney to a loved one—or a completely stranger—can open a chain that saves dozens of lives.
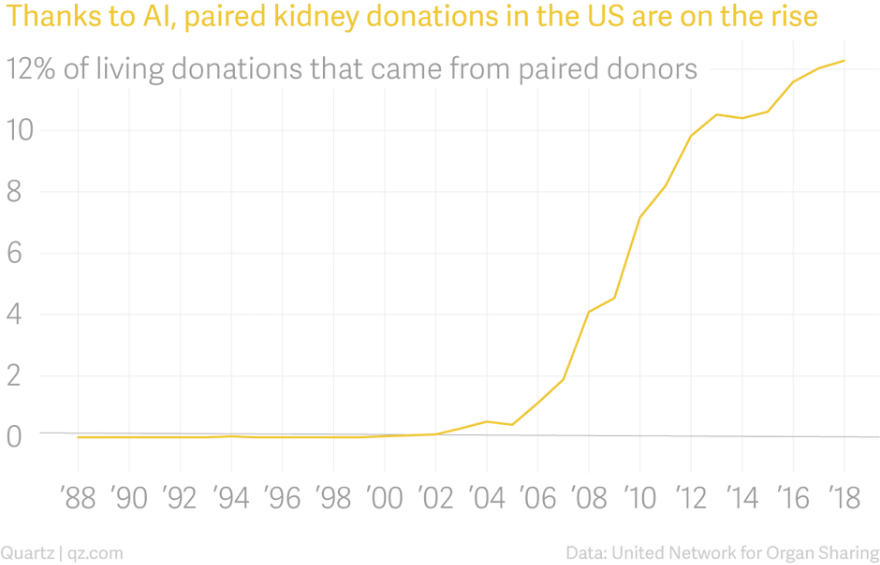
Pairing kidney donations is one of the great success stories of artificial intelligence. This does not eliminate the work, nor can it erase the human touch in health care. It deals with a very complex problem, solves it faster than humans, and has fewer errors, saving more lives. Since the first kidney exchange surgery began in 2000, nearly 6,000 people have undergone paired exchange of kidney transplants identified by algorithms. Today, about one in eight recipients of kidney transplant recipients from living donors are paired with the person through a pairing exchange.
At the same time, paired kidney exchange is also a perfect example of the limitations of artificial intelligence. Computers can only do things that humans can teach, and we can't teach things we don't understand. In the decades since the Medical Society learned how to replace kidneys with kidneys, we are still trying to solve the problem of how to distribute a small amount of precious kidneys. This distribution method makes everyone feel fair and satisfied, and does not lead to disappointment. Unexpected consequences. Artificial intelligence can identify potential donors and recipients that are biologically compatible with each other; in the future, it can even weigh the moral factors that determine who will accept the transplant first. But first, we humans must agree on what these should be.
The kidney acts as a filter for the body. For people with kidney failure, dialysis essentially replicates the function of the organ from the outside, expelling the unfiltered blood from the patient for several hours before pumping it back into the body. The invention of dialysis in the mid-20th century turned a disease that was once a death penalty into a chronic but controllable disease.
The first outpatient dialysis center, the Seattle Artificial Kidney Center, opened in January 1962. Since each patient needs two 12-hour treatments per week on the machine, the center can only accept about 2,000 of the US end-stage kidney disease patients who were eligible for dialysis treatment in the first two years.
In order to put profits in their hands, the center organized an independent committee of seven citizens. The first acceptance and policy committee – or later referred to by the media as the “God Committee†– consisted of a lawyer, pastor, banker, housewife, state government official, labor leader, and surgeon. The doctor made some decisions for them: patients over the age of 45 are not eligible, and children are not eligible because doctors worry that the surgery may bring them trauma. In addition, the committee may choose approximately one-quarter of eligible patients to apply.
According to an article in the 1962 Life magazine, the anonymous committee members will consider the age and gender of the applicant and whether they are married or have children. They will consider the applicant's emotional stability. They will look at how much money the applicant has earned and how much they have saved; their level of education, work, past behavior and future potential. They decided that since the study to develop the technology was conducted in a state-funded institution, only Washington residents would be considered because the state’s tax was paid for the treatment.
This article argues that committee members face a task that is almost impossible to accomplish as a “thinking, kind citizenâ€. They are also human beings, and as human beings, they are always influenced by conscious and unconscious prejudice. They make decisions based on the medical records written by doctors, and doctors have prejudice and unconscious bias.
The seven members of the committee are part of the upper middle class in the Pacific Northwest of the United States, and their discussions (at least those published) suggest a good impression on patients who seem to share their status and values. There is never a mention of race in Life magazine, but it's hard to imagine that in a society that is still heavily isolated (for example, 98% of Washington employees were white), people of color are not considered by these representatives. Among them.
Their discussion heralded a problem that would last long before the original kidney therapy machine was surpassed by more advanced technology. Even if a group of people unanimously promise to do the best thing possible, for most people, what is the best thing?
When the God Council issued a painful decision, other places were doing similar work to treat patients with kidney disease.
The doctor performed the first successful kidney transplant at Birgham and Women's Hospital in Boston in 1954, surgically removing an organ from a 23-year-old man and transplanting it to his twin brother. They have survived for eight more years.
By the early 1960s, the development of blood and tissue typing made it easier for doctors to identify successful matches between donors and recipients, and improvements in immunosuppressive drugs have greatly reduced graft rejection rates. Today, the kidneys of a deceased donor continue to work for 8 to 12 years in the recipient's body, while the average life expectancy of kidneys from living donors is 12 to 20 years.
In 1972, US President Richard Nixon signed legislation to expand the scope of medical insurance to include dialysis for all patients with renal failure. Dialysis did not cure them, but it allowed more people to survive longer and wait for kidney transplants. Since then, the number of people in the United States who need kidney transplants has grown much faster than the number of kidneys available.
According to the information on the Organ Sharing Network, as of this writing, 114,554 people in the United States are waiting for organ transplants. Of these, 94,980 - 83% - are waiting for kidney transplants.
The Uniform Anatomy Donation Act of 1968 established a standard procedure in the United States through which people or their close relatives could authorize the donation of their organs after death. But even though everyone in the United States is a registered organ donor (currently 54%), there are not enough kidneys to meet demand. Less than 2% of people die by making them a suitable organ donor. After a person dies, the organ can still be transplanted, and the oxygenated blood must continue to be pumped through them until it is surgically removed from the body. Before the picking operation, the deceased donor is usually declared dead and connected to the ventilator.
Fortunately, since most people have two well-functioning kidneys and only need one to survive, a living person can donate kidneys. Since living donors tend to have longer kidney life than the late ones, finding a living donor is often the ideal result for those who need to be transplanted.
Although all surgeries are at risk of complications or death, most kidney donors only need to stay in the hospital for two or three days after laparoscopic surgery, followed by another four to six weeks of recovery. The remaining kidneys will develop to compensate for the donated kidneys, and donors will usually continue to lead a normal life.
Of course, applying for an organ to your brother and sister is not a trivial matter. But finding someone who is willing to donate is usually the easiest part of the process, because many patients and their families will find it impossible to match organs.
Florida businessman Neil Emmott was diagnosed with polycystic kidney disease in 2001, a genetic disorder that could lead to kidney failure. His wife, Lisa Emmott, said the news was "unexpected and devastating." When diagnosed, Neil was 38 years old and Lisa was 27 years old. The couple had been married for less than a year. By 2016, they had two young daughters, and Neil's condition deteriorated to the point where Johns Hopkins doctors suggested that he consider transplant options.
Lisa volunteered to donate immediately. She is very healthy and has the same blood type as him, so she considers herself a viable candidate. But organ donation does not only require blood and tissue to match. A thorough screening of donors is required, and psychological or socioeconomic issues may complicate their donations. Lisa learned that a benign abnormality in her kidney artery shape—the renal artery is the vein that carries blood in and out of the kidney—has lost her qualifications. Neil's younger brother appeared as a substitute, but was also excluded because of some minor medical problems. This family is very sad.
“The need for organs is a terrible thing,†Emmott said. At this time, the family decided to seek the market.

The idea of ​​the "market" of human organs is horrifying. They are not commodities: US law expressly prohibits the sale of human organs. But from an economic point of view, the market is where anyone who wants something finds someone who can give them something. This market, which does not rely solely on price to allocate resources, is called a matching market. Dating pools are a type of matching market (assuming no money is used to exchange friendships); so are people who want kidneys and those who are willing to donate kidneys.
The market works best when the market is “thick†or has many participants. In the first few decades of kidney transplantation, sick people and their potential donors were confined to their own very weak market. A failed match is often proven to be a death sentence for a seriously ill patient.
But what if the market can get thicker?
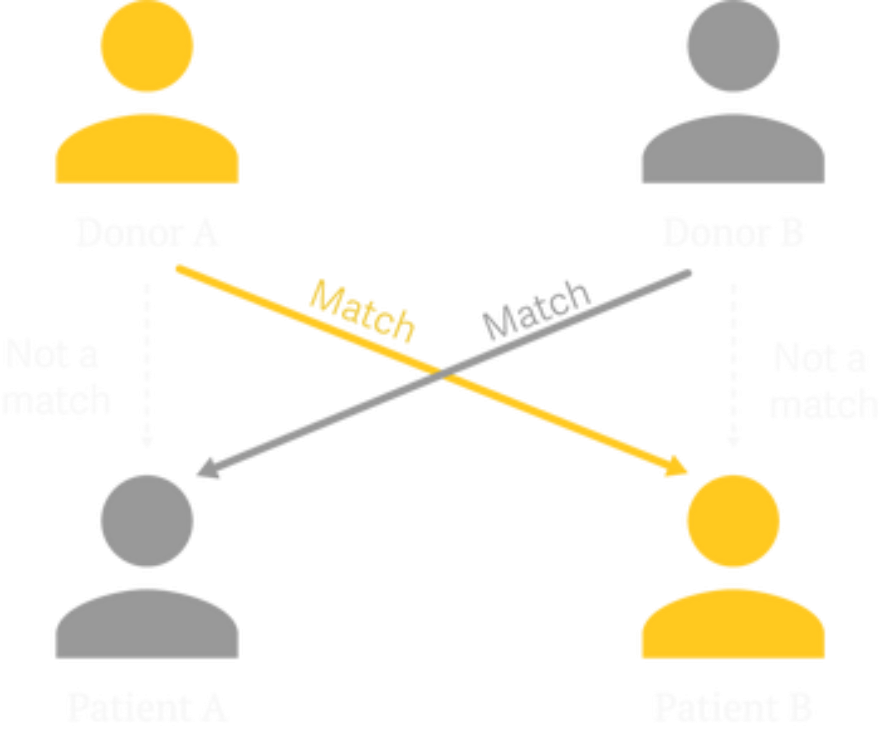
The idea was originally coined in a paper by German-American surgeon Felix Rapaport in 1986, who came up with the theory that a kidney can be transplanted across two voluntary recipients: patient A receives kidney from donor B, In exchange, donor A gave patient B a kidney.
In 1991, doctors in Seoul, South Korea, under the guidance of kidney specialist Kiil Park, performed the first kidney transplant between two donor-patient pairs. Four years later, the world's first paired kidney donation project was opened at the Yonsei University School of Medicine in Seoul. Potential donors and recipients are entered into the database and then manually paired by the doctor through hours of painstaking analysis. In 1999, Switzerland became the next country to establish a paired kidney exchange, matching two married couples, each with a spouse with end-stage renal disease and a spouse who was willing to donate the kidney.
One night in 2000, after being tired of passing heartbreaking news to patients and their loved ones, an American nephrologist named Michael Rees dragged a few boxes of documents home and spent hours checking the blood carefully. , antibody and tissue data, and compare patient lists. This work is very tiring in spirit. In the end, he realized that he didn't have a viable match—but if the donation pool was bigger, it could be paired. Working with his father, Alan Rees (Alan is a computer scientist), Michael Rees created a simple computer program that paired donors and recipients and introduced artificial intelligence into the matching process.
At about the same time, Alvin Roth, a professor of economics at Harvard University, is also working on a solution to repair kidneys. Roth focuses on market design and focuses on how to adjust the market to restore supply and demand imbalances. He has previously designed algorithms to match new doctor and residency programs, as well as New York City elementary and high school. Now he turns his attention to the kidneys.
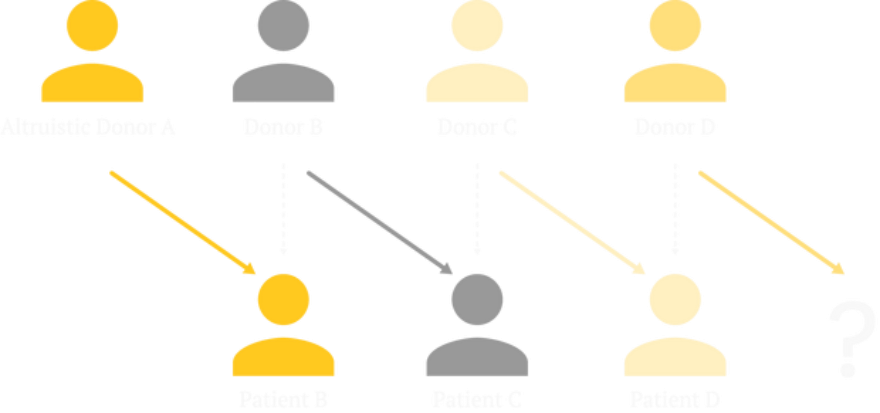
Roth and his colleagues Utku Unver and Tayfun Sonmez designed an algorithm for reviewing and analyzing data on potential donors and recipients. It identifies the “circulation†and “chain†of donor-recipient pairing, in which one chooses to selflessly donate the kidney to anyone who needs the kidney to be among potential donors and recipients registered in the hospital or kidney exchange program. A series of donations was launched. For example, Patient B gets a kidney from altruistic donor A, and then donor B gratefully donates the kidney to patient C. If Patient C has a person who is willing to donate, the chain can continue to be extended without real limitations. Unlike loops, chains can move forward indefinitely without having to go back and end the cycle by finding the kidneys for the original donor's partner recipient.
Roth, Unver and Sonmez think they are doing something big. In 2003, they published a paper on the Internet outlining their work and sent it to nephrologists across the United States. Based on feedback from Harvard surgeon Frank Delmonico, the team adjusted their algorithms and published a new paper whose concept helped establish the New England Kidney Exchange Program. The exchange program matched donors and recipients of 14 kidney transplant centers in the area.
Initially, the surgeon insists on performing all the operations simultaneously in a given cycle or chain so that no donor will retreat at the last minute. This limits the number of patients in the circulation or chain, because the hospital can only free up so many beds and so many surgeons at a time. Economists and several other doctors believe that this is an unnecessary restriction. There is no biological barrier: unlike the heart or lungs, the heart or lungs must be transplanted within 4 to 6 hours of leaving the donor's body, and the kidneys can be safely stored for 24 to 36 hours before a new host is found. As for the possibility of weak links in the donor chain, economists believe that in a chain that begins with donors willing to give kidneys to anyone, if the donors retreat, no recipient will be helpless because the doctor can Find alternatives in the Registered Donor Library.
The nephrologist Rees, who built the first matching algorithm, proved that this was achievable. After a 28-year-old donor provided a kidney to a stranger in need, Rees organized a series of kidney donations that saved the lives of 10 patients in five states over eight months.
Today, many hospitals in the United States have their own paired kidney donation programs. There are also three larger US Inter-Hospital Kidney Exchange Programs: the Joint Organ Sharing Network, the National Kidney Registry and the Paired Kidney Donation Alliance. There are national exchange programs in the United Kingdom, Canada and the Netherlands, and matching donations occur in hospitals from India to South Africa. The researchers also concluded that similar exchanges may be made between lung and partial liver transplants, although there is no such system of interchange.
In 2012, Roth won the Nobel Prize for his work in market design. He took Rees to the ceremony. By then, 2,000 people in the United States had accepted the transplant, which was the result of the system they helped create. Since then, thousands of people have been helped.
Neil Emmott eventually became one of eight people in the 2017 kidney chain, which began with a donation from two family and friends. On August 13, 2018, a woman from Alabama became the 100th person to receive a kidney transplant in the nationwide donation chain since 2013.

Today, when doctors are looking to match kidney donors and recipients, artificial intelligence researchers build algorithms to search databases of registered kidney patients and their cooperating donors, and weighted according to the Organ Purchasing and Transplant Network and the Joint Organ Sharing Network. Standard list to identify matches.
These algorithms simultaneously evaluate all possible transplants in the patient-donor library. Matching is primarily based on biocompatibility, and patients who are the most difficult to match are given priority. This technical metric includes the time the recipient is on the waiting list, his or her age (child priority), and whether the person who needs the kidney used to be a living organ donor.
These algorithms have helped thousands of life-saving surgeries. In the future, artificial intelligence can not only use human-determined criteria to match, but also actively participate in this process of judgment—understanding human decision-making and value systems, so that it can make its own judgments and decide which kidneys should go. Will be reviewed by a human doctor). At this point, the limiting factor is not so much technology, but rather the use of technology.
The first problem is human anxiety about the role of artificial intelligence in organ distribution. Hospitals and organ exchanges are even reluctant to use the term "artificial intelligence" in the matching process. Part of the reason is what researchers call the “artificial intelligence effect†trend. As Nick Bostrom, director of the Institute for Future Humanities at Oxford University, puts it, “Once something becomes useful enough and universal enough, it is no longer labeled as 'artificial intelligence'.â€
Given the lack of public education about the practical implications of "artificial intelligence," hospitals and exchanges are cautious about the role of patient misunderstanding algorithms in identifying potential matches, perhaps because of fear of juggling robots releasing cold and cold instructions.
Currently, the machine cannot decide which kidneys to go to. Humans can do this. Today's algorithms are more reliable than humans, and they perform mathematical operations on a larger scale, performing the judgments humans have made, but they don't understand why they are first calculated.
"AI doesn't have a comprehensive understanding of the world like we do. They don't understand what the data they are working on," said Vincent Conitzer, a professor of computer science, ethics and philosophy at Duke University. "They don't have the concept that this person is suffering. They don't really understand what a person is. Humans must get involved at some point."
Researchers are now teaching machines to understand these moral dilemmas from a human perspective. This year, Conitzer and Duke University colleagues Jana Schaich Borg, Walter Sinnott-Armstrong, Rachel Freedman, and John Dickerson of the University of Maryland published a paper in which they presented hundreds of hypothetical patient profiles to the subjects. Ask which of each pair should get a kidney available. These hypothetical patient profiles do not list the blood and tissue data processed by the algorithm, but rather list things such as the frequency of patients drinking and whether they have had cancer in the past. The researchers then fed back the subject's choices to an algorithm and learned how to choose the "right" kidney recipient based on these patterns. Like human subjects, artificial intelligence favors younger, healthier patients—an example of a machine that makes decisions based on an understanding of human values.
Although we can teach machines to match our value system, we don't always understand what our values ​​are, or how difficult it is to agree as a whole. People don't always know what they want to optimize, even when they think they're doing it, they often don't understand how to do it in ways that don't lead to unintended consequences.
For example, MIT's ethical machine allows visitors to the lab's website to play the games they must choose. In one hypothetical situation, the driverless car should choose which one to kill in the face of two terrible choices. Group of car passengers or pedestrians. After going through a series of nausea scenes - yes, I would rather have a car run over a pregnant woman than five homeless adults; no, if it means killing five adult passengers, I It doesn't turn abruptly to avoid two children - this game reveals the patterns it determines in your choices and how your reactions compare to the reactions of other players.
This information can reveal unexpected consequences and unpleasant unrecognized prejudice. For example, you may know that your decision disproportionately leads to more male deaths than women, or that you tend to value traffic rules more than the average player in the game.
In the kidney problem, the principle of ostensibly fairness is adopted, that is, the kidney should be given to those who may have the longest life after receiving the kidney. Before the computer can calculate the life of the potential recipient, the scientist must provide the algorithm with life expectancy data for various populations. But this has caused some problems. Men tend to die earlier than women. African Americans die earlier than Americans of any other race. In 2015, a 65-year-old white American woman may live another 20.5 years, four years longer than blacks of the same age. Although it started with good intentions, it eventually led to systematic racial and gender discrimination.
“In economics, we talk about the impossibility theorem. There are things you might want but you can't get,†Roth said. "When you allocate scarce resources, you can't give a kidney to one person without giving it to another. The computer doesn't relieve the human burden from all aspects."
Artificial intelligence does not create these moral dilemmas. The Human Committee is constantly annoyed by the fairest way to distribute the kidneys; human drivers still have to make terrible urgent decisions behind the wheel. Machines can simulate the results of human judgment in hours or even minutes, which may take years to discover. In the long run, this may help: If a computer model can prove that a particular kidney allocation policy can have a disproportionately detrimental effect on certain groups, the doctor can cancel the plan before anyone actually gets hurt. But not everyone is happy to let the machine participate in life and death.
The moral machine teaches the player something that the Seattle God Council learned a long time ago: you must choose which life to save, knowing that this decision will lead to the death or suffering of others, and it feels terrible. This part is something that artificial intelligence can't help. One can find the ideal way to assemble a chair and then pass the process on to a machine that can perfectly assemble thousands of chairs. But there is no perfect way to decide who is born and who is dead.
Heavy Biometric Safe Box,Double Door Safe Box,Combination Safe Box,Customizable Safe Box
Hebei Yingbo Safe Boxes Co.,Ltd , https://www.yingbosafes.com